Abstract
Background: High dose PT-Cy allows the safe and effective use of haploidentical relatives as an allograft source. This platform increased the pool of related donors to include haploidentical siblings, parents, and children; more recently, second-and third-degree relatives have also been shown to be safe allograft donors. There is no consensus on the ideal donor; our standard practice is to prioritize young relatives such as siblings, children, or rarely parents- is safe and feasible. AlloBMT using nonmyeloablative (NMA) conditioning is safe and feasible in select patients aged 70 and above, a large group with hematologic malignancies. An increasing number of older patients have been treated with allogeneic blood or marrow transplantation (alloBMT) using related haploidentical donors. Older patients are more likely to have older siblings and children, and recent reports associated older donor age with worse outcomes. Therefore, we report the safety and utility of grandchildren (GC) as haploidentical donors and compare outcomes to patients with children donors.
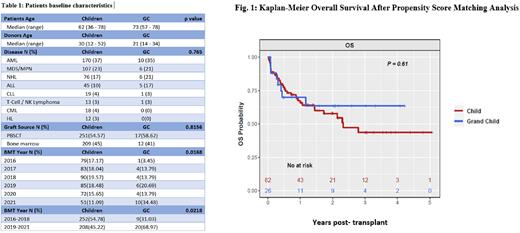
Methods: We reviewed records of patients at Johns Hopkins Hospital who received T-cell replete related allogeneic haploidentical donor blood or marrow grafts. We identified eight hundred and seven consecutive adults (≥18 years) between May 1, 2016, to October 1, 2021. Patients with aggressive myeloid and lymphoid malignancies were included. Only the first transplant was included for patients who received more than one transplant. All patients received NMA conditioning consisting of fludarabine, cyclophosphamide, and total body irradiation at 200 or 400 cGy. GVHD prophylaxis consisted of PT-Cy on days 3 and 4, followed by mycophenolate mofetil and either tacrolimus or sirolimus starting on day 5. Statistical analysis was performed using t-test, Wilcoxon rank sum test, or Chi-square test. Overall survival (OS), progression-free survival (PFS), relapse and non-relapse mortality (NRM) were estimated using Kaplan-Meier methods. Additionally, propensity score matching analysis (PSMA) for patient's age, BMT year, and graft source was performed.
Results: Analysis was done on four hundred and sixty patients who received grafts from children donors and twenty-nine grandchildren donors. The median follow-up for patients was 28.8 (range 0.2 - 70.8) and 30 (range 0.8-50.4) months in children and GC, respectively. The most common diagnosis in both groups was acute leukemia compromising about a third of the patients, followed by myelodysplastic syndrome/ myeloproliferative disorders and Non-Hodgkin's (Table 1). Median age of patients in the GC group was 11 years older, 73 years (range 57-78) compared to 62 years (range 36 - 78) in the children group. The median age of children donors was 30 years (range 12-52), and 21 years (range 14-34) in the GC group.
Patients in the GC group had higher comorbidities compared to patients in the children group, with a median hematopoietic cell transplantation comorbidity index (HCT-CI) of 2 (range 1-5) and 1 (range 0-7) respectively, (P=0.001). There was almost twice as many patients with HCT-CI of ≥3 in the GC compared to the children group, 38% and 21% respectively. The use of marrow vs PBSC as the graft source was not significantly different between the two groups (table 1).
The two-year cumulative incidence of NRM was statistically significant higher for the GC group at 27% compared to 12% in the children group (P= 0.02). Since NRM is more likely in older patients, and older patients were more likely to be in GC group, we performed a PSMA. When matched for age, BMT-year and HCT-CI, PSMA did not show significant differences in NRM (HR 1.49, 95% 0.7-3.4, P=0.35). Similarly, OS, relapse and PFS did not show differences before or after PSMA. The two-year OS was 58% and 64% for children and GC, respectively (HR 0.82, 95% CI 0.36-1.88, P=0.63). Two-year relapse cumulative incidence was 24% and 7% for children and grandchildren, respectively (HR 0.45, 95% CI 0.15-1.34, P=0.15). Two-year PFS was comparable 52% and 56% for children and GC groups, respectively (HR 0.93, 95% CI 0.5-1.73, P=0.82) (fig. 1).
Conclusions: Despite older age and comorbidities, the outcomes of alloBMT from grandchildren were at least as good as those from children, with 2-year OS of 64% and 58%, respectively. Choosing grandchildren as donors was associated with promising outcomes and should be examined further.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal